 The cost of physician burnout is real and tangible. When physicians burn out, patients are less likely to be satisfied with their care and less likely to adhere to medical advice. Healthcare organizations lose millions of dollars annually to physician burnout. And burned out providers are more likely to succumb to alcohol abuse and dependence, as well as suicidal ideation – a critical issue at a time when suicide rates in the U.S. are climbing dramatically.
The cost of physician burnout is real and tangible. When physicians burn out, patients are less likely to be satisfied with their care and less likely to adhere to medical advice. Healthcare organizations lose millions of dollars annually to physician burnout. And burned out providers are more likely to succumb to alcohol abuse and dependence, as well as suicidal ideation – a critical issue at a time when suicide rates in the U.S. are climbing dramatically.
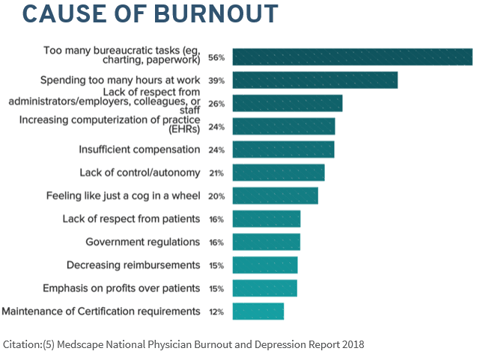
When asked why they’re burned out, physicians cite the same causes repeatedly: Too many bureaucratic tasks. Too many hours at work. Not enough respect from administrators, colleagues, and staff. And, as has been written about many times before, the increasing pressure to master the EHR.
We’ve talked before about our belief that the EHR is a symptom, not a cause, of physician burnout. Today, we’d like to talk about a few simple things that can be done to help providers see the EHR as a means of solving burnout rather than a contributing factor.
Turning the EHR into a helpful tool
Because many physician tasks, such as documentation and chart review, take place in the EHR, it can be easy to see the EHR as the cause of burnout. But in fact, the real source of burnout comes from increased regulatory and documentation requirements, not from the system itself.
The key to decreasing burnout is to optimize providers’ use of the system through a combination of personalization and training. According to statistics from the KLAS Arch Collaborative, training is the No. 1 predictor of physician satisfaction with the EHR, closely followed by personalization.
So what do we mean by training and personalization? You can think of the EHR the same way you’d think of any other technology you use on a daily basis, such as your smartphone.
When you first bought a smartphone, it was probably a little overwhelming – you didn’t know where anything was, and it seemed to take twice as long to find someone’s phone number or open the camera app. But over time, someone showed you how to use voice-activated text, and you started arranging programs to work the way you wanted them to (for example, to program your alarm for the same time every day or to show certain numbers as your favorites).
Once you were trained to use your phone and had personalized its features to fit your lifestyle, it probably felt much, much easier to manage your daily life.
The same is true of the EHR. Our optimization implements training and personalization by using a data-driven approach to understand physician behavior:
1. Use data to tailor intervention.
We start with a dashboard that pulls in data on system usage and shows you where providers are struggling and succeeding in the system. For example, the dashboard might show that a certain department is spending more than the average amount of time in chart review after hours, suggesting a higher likelihood for burnout. We can drill down to the department level, specialty level, and provider level to make sure that those struggling are getting the attention they need and that we can learn from successful providers as well.
2. Communicate thoughtfully with providers.
Armed with data, we encourage trainers to have honest, empathetic conversations with providers about how they’re using the system. Data doesn’t tell the whole story, but it can give you a valuable starting point to have a conversation about where someone is struggling. Sit down with providers, share your data, and give them a chance to reflect.
3. Find opportunities for personalization within the system.
Getting physicians to use personalization features is absolutely critical in increasing system efficiency. According to KLAS, “Use of personalization settings has a dramatic effect on user experience, yet fewer than half of the personalization options that users have are actually being utilized.” Personalization features like Preference Lists, Quick Actions, and Express Lanes can significantly decrease the amount of time providers spend in the system by automating common tasks.
4. Conduct at-the-elbow training.
We’ve found that organizations get the most bang for their buck when they conduct at-the-elbow retraining on provider “quick wins.” Have your trainers sit with physicians and walk them through how to use personalization features, ensuring that mistakes and confusion are tackled as soon as they arise.
***
One of the most important recommendations we can give is to frame training and personalization as a way to help providers save time and feel less stressed. If physicians feel targeted or scolded for their lack of mastery, they may hesitate or flat-out refuse to take part in retraining. Instead, ask, “What would you do with an extra five minutes per hour?” and let that guide your conversation about using the system more efficiently.
We also recommend assigning a physician to teach your classes, standardizing your curriculum, and grouping specialties together to make the classes feel more personalized. The more you can show your physicians that you’re there to help and understand their needs, the higher rate of training compliance you’ll be able to achieve.
