I work for a healthcare company. People might think that I work for a consulting firm that does healthcare, but we at Nordic see it differently. We’re a healthcare company that happens to do consulting (and managed services and staffing and other things, but I digress). First and foremost, we’re a healthcare company.
As a physician working at a healthcare company, I am often asked about medical issues that need to be addressed as part of our work. In addition, though, I sometimes hear from our employees about their own personal medical adventures. Often, the refrain is, “Can I run something by you? Does this seem normal? What would you do in this case?” With the permission of one such employee and the certainty that no privacy rules have been broken, allow me to tell you a healthcare story.
I’ll call this employee Juan (not their real name). Juan’s mom was in the hospital with breathing problems due to chronic disease. As is now typical in the United States, she was being cared for not by the primary care doctor who she saw regularly in the clinic, but by a group of specialists who focus on inpatient hospital care. Hospitalists (you saw that coming, didn’t you?) typically work 12-hour shifts for perhaps a week in a row, and usually follow the same group of patients while they’re on service. One of the benefits of hospital medicine is that these physicians become quite good at learning how a specific hospital runs its lab, how its electronic health record (EHR) works, and how its staff interacts.
One of the great aspects of hospital medicine is that it allows doctors to work set shifts. This makes it possible for physicians to actually have a life outside of medicine and focus on their families, friends, and themselves. But one of the realities of shift work is that communication among the clinical team becomes even more essential than ever. One physician must pass on to their colleague coming into the hospital all that has transpired since they left the hospital. This “dance” requires coordination, planning, and consistency. Further, this focuses just on the primary care team; keeping all of the specialists coordinated and in the loop requires even more work. The EHR is typically the center of the universe for all clinical data, but sometimes, even it’s not enough.
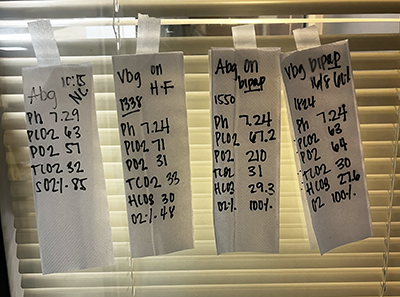 As Juan’s mom was not improving, different methods of non-invasive ventilation were being leveraged. She tried nasal canula (NC) oxygen, high frequency (HF) ventilation, and bilevel positive airway pressure (BiPAP). As her doctors were worried about her, they ordered frequent blood tests to judge the levels of oxygen and carbon dioxide in her system. How did the team judge her progress from the blood gas results? A nurse or respiratory technologist wrote them down on paper towels and taped them to the window.
As Juan’s mom was not improving, different methods of non-invasive ventilation were being leveraged. She tried nasal canula (NC) oxygen, high frequency (HF) ventilation, and bilevel positive airway pressure (BiPAP). As her doctors were worried about her, they ordered frequent blood tests to judge the levels of oxygen and carbon dioxide in her system. How did the team judge her progress from the blood gas results? A nurse or respiratory technologist wrote them down on paper towels and taped them to the window.
At first glance, this seems … incredible. Why would this be necessary in a modern healthcare facility that is likely using a state-of-the-art EHR? (For the record, I don’t know the vendor that this hospital used.) The EHR and lab systems were up and running according to Juan, so a technical glitch can be eliminated. What else could have led to this window “art?” I have some educated guesses.
It seems that Juan’s mom was struggling a bit, so her doctors were trying different tools to ease her respiratory efforts. In a fast-changing environment, team members may not be up to date with current decision making. If you weren’t aware that the patient had been changed to a different modality or that frequent blood gas tests were being performed, then it’s reasonable to assume that you weren’t checking on those results. By writing key aspects of the blood gas results as well as associated ventilation settings (context is essential) on paper towels and taping them in a prominent part of the patient’s room, it would be almost impossible to miss some of the critical pieces of information needed to care for Juan’s mom.
It’s also possible that the EHR or other electronic system used to find the lab results presented them in a way that made interpretation or trending difficult. How would that work? I’ve seen some things; let me throw out some options. As I wrote in the last paragraph, for many test results, context is key. For instance, looking at the blood pH or pO2 by itself is fairly useless. Clinicians need to know what breathing assistance was being used at the time to properly interpret the results and draw conclusions as to what’s next for the patient. So, if the results were presented on one screen and the doctor had to go to another screen to see what sort of support the patient was getting at the time, I see the utility of the paper towels.
Another potential problem could be how the EHR presented the data. Most clinicians are accustomed to seeing certain data in a reproducible and common way. Want to know how the patient team caring for Juan’s mom expected to see these blood gas results? Look no further than the paper towels taped on the window. It’s possible that the tech the hospital used presented the results in a different order (alphabetical?) or a different format (horizontal?).
In either scenario, clinicians would likely be crying out for order from the chaos.
Human-centered design requires predictability. Clinicians have generated muscle memory by looking at results in a particular way throughout their training and practice. When non-clinicians try (either purposefully or accidentally) to change the way doctors experience healthcare data or interactions, we’re moving in the wrong direction. Perhaps there was no good alternative to the paper towels being taped on the window, but … that’s not what windows are for, and there is opportunity to do better.